Age-related macular degeneration
It is the number one cause of irreversible visual loss in people over 50 years age in the United States and western Europe. The risk of macular degeneration increases with age, family history, light iris color, smoking, hypertension, and high cholesterol.
There are two types of macular degeneration, dry and wet.
Dry macular degeneration: 80% of patients with macular degeneration have dry type. The macula, the central area of the retina used for the sharpest vision, develops small round yellow deposits known as drusen. These deposits are made up of undigested cellular materials, lipids, and proteins. There is also premature loss or abnormal proliferation of retinal pigment cells which helps maintain retina. Drusen and pigment abnormalities cause progressive damage to the photoreceptors of the retina, resulting in visual deterioration.
While there is no cure for dry macular degeneration, recent national studies have shown benefits of certain nutritional and dietary intakes.
- Vitamin C, Vitamin E, Beta carotene, Zinc, and Copper: Age -Related Eye Disease Study showed that people with moderately severe dry macular degeneration may reduce the risk of their disease progression by 25 percent by taking 500mg of Vitamin C, 400 IU of Vitamin E, 80 mg of zinc oxide, 2 mg of cupric oxide daily, and 10 mg / 2 mg Lutein / Zeaxanthin.
- Consumption of dark leafy vegetables and oily fish.
- Treat hypertension and cholesterol.
- Avoid smoking.
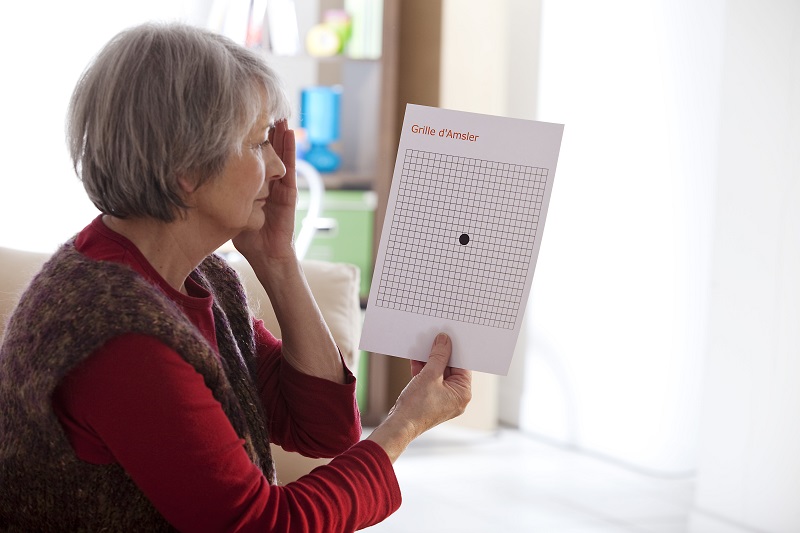
It is important to know that people with dry macular degeneration are at risk for developing wet macular degeneration, which can cause rapid loss of central vision but has possible beneficial treatment. Patients with dry macular degeneration are therefore encouraged to monitor their vision daily with Amsler grid as well as undergo regular dilated retinal examination.
Wet Macular Degeneration: This type of macular degeneration is distinguished from the dry type by the presence of abnormal blood vessels underneath the retina, known as choroidal neovascular membrane. These abnormal blood vessels grow through the cracks that develop in the tissue layers below the retina and eventually form permanent scars, resulting in the damage to the photoreceptors. Patients who develop wet AMD complain of sudden onset of visual deterioration, distortion, and/or blind spot. Dilated retinal exam is needed to detect evidence of abnormal vessels, which is often accompanied by the presence of visible fluid, lipids, and hemorrhages. Special tests such as fluorescein angiography and optical coherence tomogram are performed to aid the diagnosis.
Based on the examination findings, the doctor can determine whether any treatment can be beneficial to stop the abnormal blood vessels. Since the blood vessels form a permanent scar tissue, it is helpful to detect the disease process as early as possible.
Possible treatments include:
- Intravitreal injection of Avastin, Lucentis, Vabysmo, Eylea and Eylea HD: These drugs have special properties in stopping new blood vessel formation and are injected directly into the inside cavity of the eye at periodic intervals, as determined by the patient’s response.
- Laser: A beam of laser light is used to coagulate the diseased tissue.
- Photodynamic therapy: Photosensitizing dye is given intravenously and a non-thermal laser is then applied to the diseased tissue with minimum damage to the healthy retinal tissue.
- Your retinal specialists will determine which treatment will be most appropriate for you.