Retinal Disease Care in Las Vegas, NV
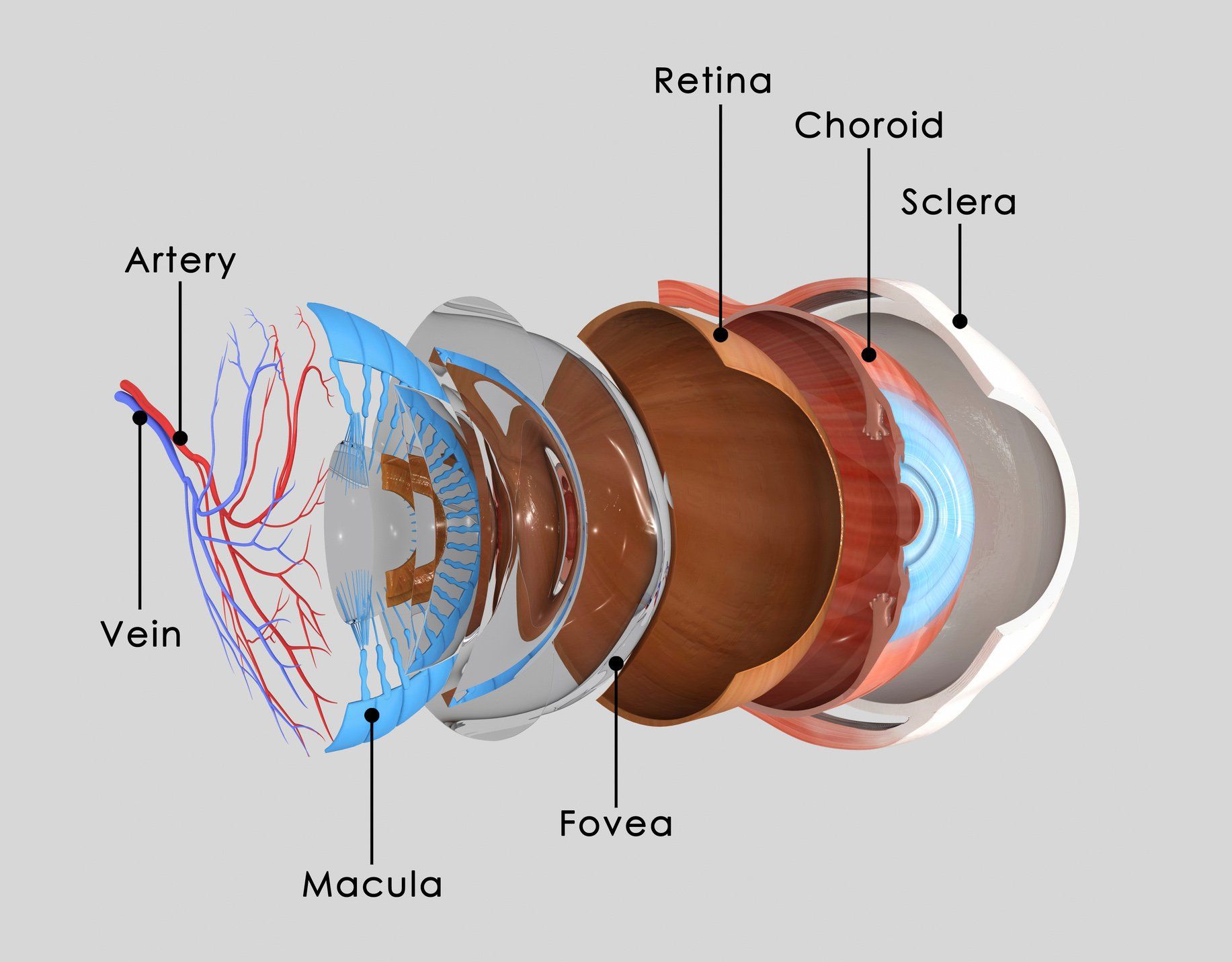
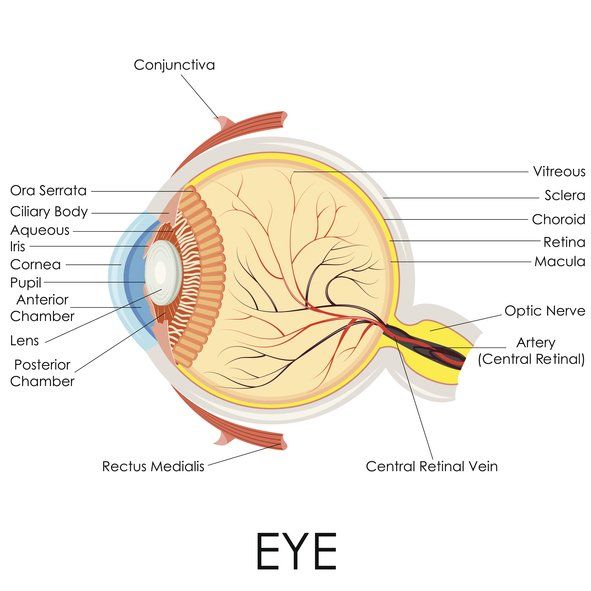
Eye Anatomy
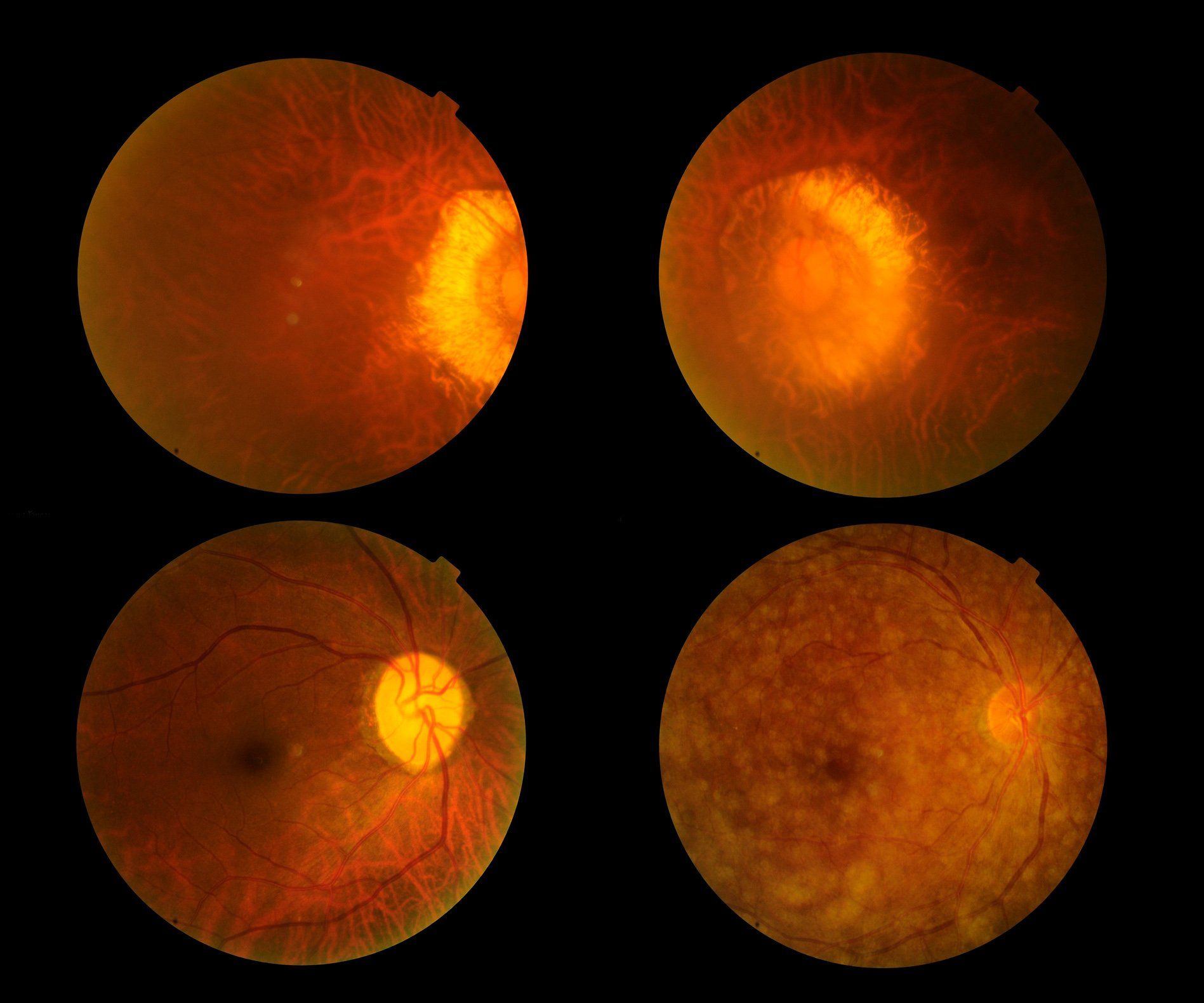
Macular Degeneration
While there is no cure for dry macular degeneration, recent national studies have shown benefits of certain nutritional and dietary intakes.
- Vitamin C, Vitamin E, Beta carotene, Zinc, and Copper: Age -Related Eye Disease Study showed that people with moderately severe dry macular degeneration may reduce the risk of their disease progression by 25 percent by taking 500mg of Vitamin C, 400 IU of Vitamin E, 80 mg of zinc oxide, 2 mg of cupric oxide daily, and 10 mg / 2 mg Lutein / Zeaxanthin.
- Consumption of dark leafy vegetables and oily fish.
- Treat hypertension and cholesterol.
- Avoid smoking.
It is important to know that people with dry macular degeneration are at risk for developing wet macular degeneration, which can cause rapid loss of central vision but has possible beneficial treatment. Patients with dry macular degeneration are therefore encouraged to monitor their vision daily with Amsler grid as well as undergo regular dilated retinal examination.
Wet Macular Degeneration: This type of macular degeneration is distinguished from the dry type by the presence of abnormal blood vessels underneath the retina, known as choroidal neovascular membrane. These abnormal blood vessels grow through the cracks that develop in the tissue layers below the retina and eventually form permanent scars, resulting in the damage to the photoreceptors. Patients who develop wet AMD complain of sudden onset of visual deterioration, distortion, and/or blind spot. Dilated retinal exam is needed to detect evidence of abnormal vessels, which is often accompanied by the presence of visible fluid, lipids, and hemorrhages. Special tests such as fluorescein angiography and optical coherence tomogram are performed to aid the diagnosis.
Based on the examination findings, the doctor can determine whether any treatment can be beneficial to stop the abnormal blood vessels. Since the blood vessels form a permanent scar tissue, it is helpful to detect the disease process as early as possible.
Possible treatments include:
- Intravitreal injection of Avastin, Lucentis, Vabysmo, Eylea and Eylea HD: These drugs have special properties in stopping new blood vessel formation and are injected directly into the inside cavity of the eye at periodic intervals, as determined by the patient's response.
- Laser: A beam of laser light is used to coagulate the diseased tissue.
- Photodynamic therapy: Photosensitizing dye is given intravenously and a non-thermal laser is then applied to the diseased tissue with minimum damage to the healthy retinal tissue.
- Your retinal specialists will determine which treatment will be most appropriate for you.
Diabetic Retinopathy
Diabetic retinopathy is the number one cause of visual loss in patients aged 20-64 years in the United States. It is caused by hyperglycemia(high blood sugar) induced damage to the tiny blood vessels in the retina. The risk of diabetic retinopathy is closely related to the duration of diabetes, control of blood sugar, and associated medical conditions such as hypertension, kidney, and heart disease. In its early stages, diabetic retinopathy cause very little visual symptoms if any, causing a delay in patients seeking eye care. Patients often have advanced disease stage by the time they come to the doctor's office with visual symptoms. In addition, many patients do not have optimal sugar control for a variety of reasons contributing to severe and rapid progression of the disease despite treatment. It is there imperative for anyone with diabetes to have a regular dilated retina evaluation to detect diabetic retinopathy as early as possible and maintain best possible blood sugar control.
There are two clinical stages of diabetic retinopathy:
• Nonproliferative diabetic retinopathy: Patients develop tiny hemorrhages, microaneurysms, and leakage of fluid from the damaged blood vessels.
• Proliferative diabetic retinopathy: Abnormal new blood vessels form on the surface of the retina, causing hemorrhage and retinal detachment.
Patients with either clinical stage of diabetic retinopathy may develop macular edema. Macular edema results when the center of the retina, called macula, develops swelling from the leaking blood vessels. The swelling of the macula leads to dysfunction of the photoreceptors and resultant blurred vision.
Medical management of diabetic retinopathy: The most important factor in the medical management of diabetic retinopathy of course is to maintain good blood sugar control. The Diabetes Control and Complications Trial showed that intensive control of blood glucose is associated with reduced risk of newly diagnosed diabetic retinopathy and reduced progression of existing diabetic retinopathy. The United Kingdom Prospective Diabetes Study also showed that the control of hypertension was also beneficial in reducing the progression of diabetic retinopathy and loss of vision.
Laser treatment of Diabetic Retinopathy: Laser is an intense focused beam of light of certain wavelength that can be used to photocoagulate tissues. It is used to prevent further growth of abnormal blood vessels in proliferative diabetic retinopathy and to stop leaking blood vessels to prevent macular edema. Several national studies have clearly demonstrated the effectiveness of laser treatment in reducing the risk of developing severe visual loss. It is the primary treatment used by retinal specialists for diabetic retinopathy. There are certain criteria used in deciding when the laser treatment is appropriate for a given patient based national studies. This determination requires dilated retinal examination, and sometimes special diagnostic tests such as fluorescein angiogram. The location and the size of retinal swelling relative to the center of the retina, as well as the presence of hemorrhages within the vitreous cavity and the size of the abnormal blood vessels, are the major determinants of whether a laser treatment is warranted. Panretinal laser treatment is used for proliferative diabetic retinopathy, whereas macular laser treatment is used for macular edema. Panretinal laser is applied to the peripheral retina in a scattered fashion to reduce the area of diseased retina, which helps discourage the growth of abnormal blood vessels. Macular laser is applied directly to the leaky blood vessels to prevent continued leakage, which helps prevent macular edema. Panretinal laser can reduce the rate of severe visual loss by 50% or more. Macular laser can reduce the rate of moderate visual loss by 50%.
Intraocular Injection for Diabetic Retinopathy:
- Intravitreal anti-VEGF drugs: Avastin, Lucentis, Vabysmo, Eylea and Eylea HD are agents given by injection to treat macular edema.
- Intravitreal steroid injection: Administration of intraocular corticosteroids such as Kenalog or Ozurdex, can reduce macular edema.
- Par plana vitrectomy: This is an operating room surgical procedure performed in the setting of severe diabetic retinopathy. The indications for the procedure include non-clearing severe vitreous hemorrhage, retinal detachment, and diffuse macular edema, which have not responded to other treatment modalities. The procedure involves making three tiny incisions into the vitreous cavity. Special microinstruments are inserted through the incision to remove blood and scar tissues, apply laser, and perform other necessary steps.
Since diabetic retinopathy is caused by a systemic disease associated with high blood glucose, the prognosis for diabetic retinopathy in a given patient ultimately depends on how well he or she controls her diabetes. Please ask and get help from your doctor. Please have regular examinations, keep your hemoglobin A1C below 7, control your blood pressure and cholesterol, and check for any heart or kidney diseases. Please have your retina examined regularly with dilation to detect and treat diabetic retinopathy.
Floaters & Flashes
Floaters are any number or shapes of moving dots, spots, or lines in our vision due to opacities inside the vitreous cavity. The most common cause of floaters is vitreous detachment. In vitreous detachment, the vitreous, the gel inside the back of the eye, undergoes age-related thickening, which causes it to suddenly start separating from the retina, the inside lining of the eye. This phenomenon also can cause the visual sensation of bright light, referred to as flashes. The vitreous gel separation can sometimes result in a retinal tear, which can lead to retinal detachment and loss of vision. If you experience sudden onset of new floaters or flashes, or increase of them, you are recommended to contact your retinal specialist urgently to have a dilated retinal examination to detect retinal breaks or detachment.
Vein Occlusion
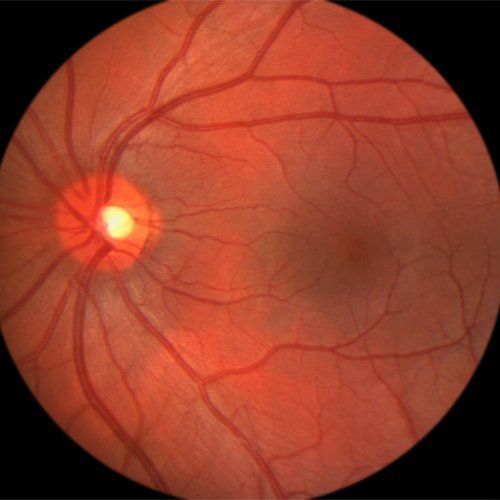
Retinal veins drain blood from the retinal arteries and capillaries and send it back to the heart. Retinal vein occlusion occurs when a retinal vein becomes blocked. The blockage leads to the poor blood flow and damage to the blood vessel walls, causing the blood and the fluid to leak into the retina and damage the photoreceptors essential for normal vision.
Retinal Detachment and Tear
The retina, which is a thin membrane lining the inside wall of the eye, converts focused light into electrical impulses that are transmitted to the brain via optic nerve for vision to take place. Sometimes, the retina can develop a break and detach from the underlying eye wall, which leads to visual loss. A retinal break can happen either spontaneously in certain predisposed person such as a person who is very near sighted or with family history of retinal detachment, or in rare cases following severe direct eye trauma. However, the most common cause of a retinal break is a vitreous detachment, which occurs when the gel inside the eye undergoes natural degeneration and becomes thicker, causing it to separate from the retina. Vitreous detachment happens to everybody some point in time. Since the retina is so thin, the separating gel can tear the retina in certain predisposed person. When the liquid inside the eye starts to leak through the retinal break and collects under the retina, the retinal detachment can starts to form. During the early stage of retinal detachment, there may not be any noticeable symptom. When the area of retinal detachment becomes larger, the affected person can notice a curtain or shadow, which progressively enlarges. Since onset of floaters or flashes may be a warning sign of possible retinal tear that can lead to retinal detachment, it is highly recommended to have a dilated retinal examination when you are having new floaters as soon as possible.
Treatment
- Retinal breaks: The most common treatment is laser photocoagulation with laser. The laser beam is placed around the retinal break to form an adhesion to prevent the retina from detaching. This is usually performed in an office setting and, in most cases, highly successful. In some cases, especially if blood is present to prevent laser uptake, cryotherapy is performed to freeze the area around the retinal tear to achieve the same effect.
- Retinal Detachment: If the retina is already detached to a certain degree, laser is no longer applicable. In this case, surgery is needed. Types of retinal detachment surgical technique is dependent upon several factors including location and size of the retinal tears, duration of retinal detachment, and presence of retinal scars. Mainly, there are three techniques: pneumatic retinopexy, scleral buckle, and vitrectomy. Sometimes, combination of these techniques are used to repair a given retinal detachment.
Uveitis
Uveitis is defined as inflammation of the uvea, which consists of the iris, ciliary body, and the choroids. There are many different causes of uveitis including infection, trauma, neoplasm, or autoimmune diseases.
Signs and symptoms
The most common presenting symptoms include blurred vision, pain, light sensitivity, redness, and floaters. The signs of uveitis depend on the cause and location of predominantly affected area inside the eye. Examination may reveal deposits of inflammatory cells on the cornea, iris, lens or vitreous cavity. It may also show swelling in the retina and leakage around the retinal blood vessels.
Classification of uveitis
Uveitis is classified into four major types depending on the location of inflammation
- Anterior uveitis: inflammation is present mostly in the anterior chamber and the iris of the eye. Possible causes include HLA-B27 associated diseases, idiopathic, JRA, herpes simplex, sarcoidosis, and trauma.
- Intermediate uveitis: inflammation is present in the middle part of the eye. Possible causes include idiopathic, sarcoidosis, and multiple sclerosis.
- Posteriror Uveitis: Inflammation primarily involves the back of the eye. Common causes include infectious processes such as parasites, bacteria, virus,
sarcoidosis, idiopathic and autoimmune reaction.
Epiretinal Membrane
An epiretinal membrane (ERM) is a thin transparent tissue that forms on the surface of the retina. The membrane can be secondary to:
- Spontaneous separation of vitreous gel inside the eye
- Wide variety of conditions such as blood vessel damage, inflammation, trauma, surgery, and retinal breaks.
Approximately 2% of patients over 50 have ERM.
Signs and symptoms
An ERM is usually located in the center of the retina, the macula. In early stages, the membrane is thin and difficult to detect with very little, if any, symptoms. Over time, the membrane may become thicker, which then cause the underlying retina to become distorted and wrinkled. Further changes can lead to swelling, hemorrhage, and even detachment of the retina. Symptoms include decreased vision, distortion, wavy lines, and double vision. In many patients, however, the ERM can remain stable for a long time without much change in vision. Diagnosing ERM requires a dilated retinal exam along with special testing such as fluorescein angiogram and optical coherence tomogram.
Treatment
Most patients have mild symptoms and do not require treatment right away. For patients with significant symptoms, surgical removal of the ERM may be indicated. Pars plana vitrectomy is the surgical technique used to peel the ERM by making micro-incisions into the vitreous cavity and using a variety of instruments to remove the membrane from the surface of the retina. It is performed in the operating room, either under local or general anesthesia.
Macular Hole
A hole can spontaneously develop in the center of the macula, causing loss of central vision. It occurs usually in the sixth through eighth decades of life. The etiology of the hole is thought to be related to the tractional forces associated with vitreous gel separation that occurs naturally. Retinal exam and optical coherence tomogram are used to diagnose and stage the hole. The formation of macular hole goes through several stages:
- Stage 1: Patients experience onset of visual symptoms with distortion and decreased vision. Exam reveals evidence of cystic elevation in the center of the macular causing a tiny circular yellow spot with a full thickness hole.
- Stage 2: A full thickness defect start to develop as a break forms in the roof of the cyst further deterioration of vision.
- Stage 3: A fully developed hole is present along with a rim of subretinal fluid. The vitreous gel is still attached to the macula.
- Stage 4: The hole is fully developed and the vitreous gel has become detached from the macula.
Treatment
Patients with a stage 1 hole are usually observed, as approximately 50% of the patients may experience spontaneous resolution according to some studies. However, most patients with more advanced stage 2- 4 macular hole do not improve and should consider vitrectomy. The surgery is performed by removing the gel and injecting gas bubble into the vitreous cavity. The patient is required to maintain his/her face down up 1 to 2 weeks to allow the gas bubble to be in contact with the hole and allow the hole to close. The rate of success can be as high as up to 70 to 90% in closing the hole and improving the vision.